When it comes to breast cancer, sometimes the biggest advantage is simply knowing your risk.
Genetic testing can give women that head start and for two South Florida survivors, those results helped them face a devastating diagnosis head-on.
Cancer is a six-letter word that sparks fear for many
In 2025, roughly two million people in the United States are expected to be diagnosed with some form of the disease.
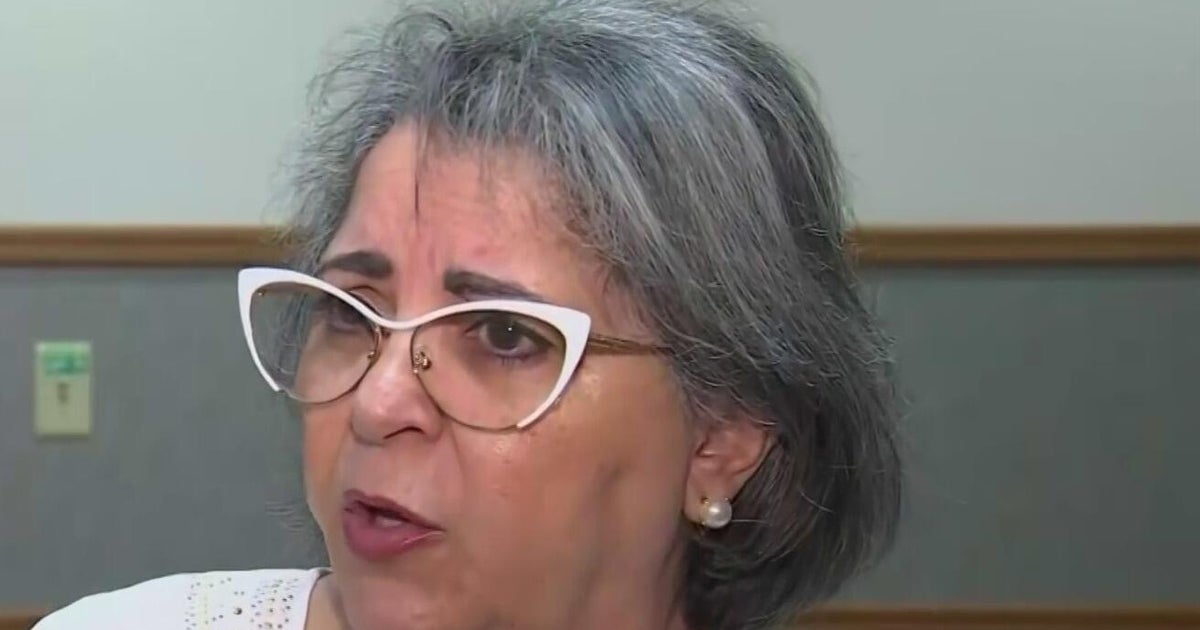
For Marie Montelongo, her story began with her mother. “At age 73, she was diagnosed with breast cancer, and she passed away at age 79,” Montelongo said.
Years later, Montelongo faced breast cancer herself.
“I was very concerned for my daughter and my granddaughter and the future, thinking I might have something that I could pass on to them. So, I asked for the genetic testing,” she said.
Tammy Adar, a genetic counselor at Memorial Cancer Institute, says testing can be an important tool for both patients and their families.
“Genetic testing can be important to know what somebody’s risks are,” Adar said. “If someone has cancer, we may need to know if they have risks for additional cancers—or if someone with a family history may be at increased risk.”
The test itself is simple: usually one or two tubes of blood or a saliva sample sent to a lab, with results available in two to three weeks. It’s typically covered by insurance but can also be done out of pocket for around $250.
Making treatment decisions: When results guide surgery choices
Montelongo’s results came back negative, but that raised more questions. “Like where did my breast cancer come from?” she said.
Still, she and her doctors made a plan. Because of her family history, she opted for a double mastectomy. Today, she’s cancer-free.
For Alvette Randoe, the path was even tougher. She was diagnosed with stage two breast cancer that had already become metastatic. Her mother died of the disease when Randoe was six, and her sister battled both breast and ovarian cancer and survived.
“I wanted to save my life,” Randoe said.
Doctors recommended full genetic testing because her risk for the BRCA gene mutation was 91%. Randoe underwent both a mastectomy and a hysterectomy. Today, there is no longer cancer in her body.
“You don’t want to not know any results,” she said. “You want to have a fighting chance.”
Early detection and family history key to fighting cancer
Adar says that’s exactly the purpose of testing.
“If we know someone is at increased risk, we can do additional or earlier screenings so that we can catch cancer early, better treat it, and better cure it,” she said.
Both women continue regular checkups and monitoring, but most importantly, they get to live.
“You never really live without the fear of it coming back,” Montelongo said. “But every year when I do my scans and they come back normal, it’s a sigh of relief.”
For Randoe, there’s no question she made the right decision.
“It’s been a long road,” she said. “But is it worth it? A thousand percent.”
Doctors stress that routine screenings and knowing your family history remain the best ways to catch cancer early and save lives.